Age | Family history | Hereditary risk | Genetic inheritence | Lynch syndrome | FAP | MAP | Crohn's disease | Ulcerative colitis
Anything that increases your chance of developing bowel cancer is called a cancer risk factor. Some risk factors can be avoided, but many cannot.
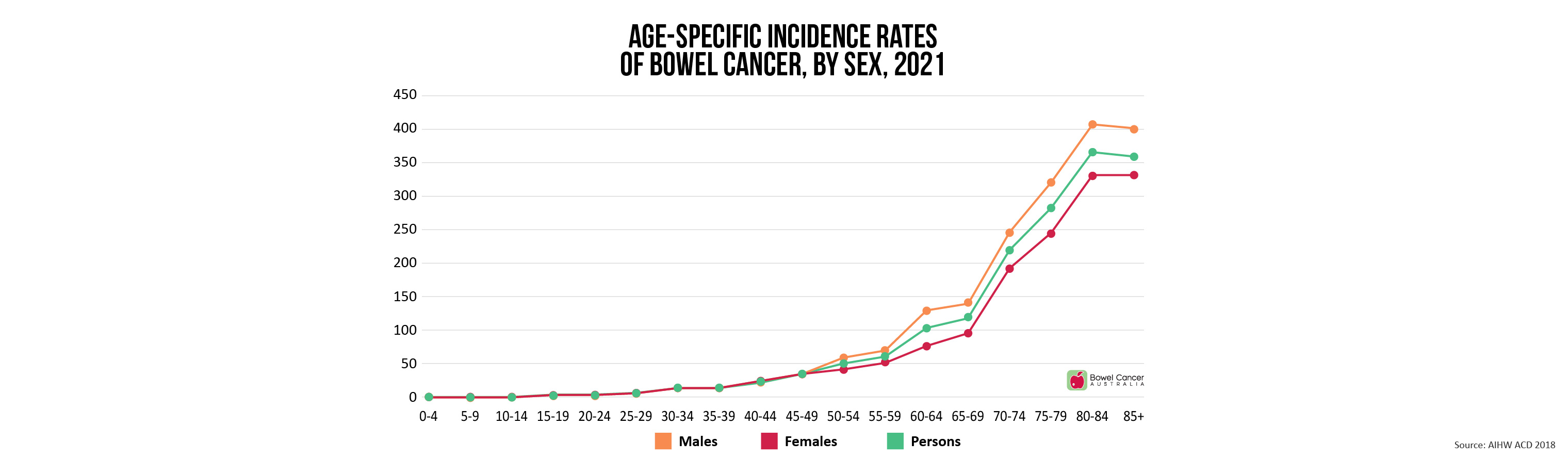
- Age - bowel cancer risk increases with age. Incidence begins to increase significantly between the ages of 40 and 50, and age-specific incidence rates increase in each succeeding decade thereafter (i.e. 50-60; 60-70; 70-80 etc). Although bowel cancer is less common among younger adults, rates are on the rise, with 1-in-10 bowel cancer cases now diagnosed in Australians under age 50.
- A family history of bowel cancer
- A personal history of cancer of the colon, rectum, ovary, endometrium, or breast
- A history of polyps in the colon
- A history of ulcerative colitis (ulcers in the lining of the large intestine) or Crohn's disease
- Hereditary conditions, such as Familial Adenomatous Polyposis (FAP) and Hereditary Non-Polyposis Colon Cancer (HNPCC; Lynch Syndrome).
About 70% of people who develop bowel cancer have no family history of the disease.
However, for around 30% of all bowel cancer cases diagnosed there is a family history, hereditary contribution or a combination of both.
Generally speaking, the more members of the family affected by bowel cancer, and the younger they were at diagnosis, the greater the chance of a family link.
Genetic mutations have been identified as the cause of inherited cancer risk in some bowel cancer–prone families; these mutations are estimated to account for only 5% to 10% of bowel cancer cases overall.
| What is my risk of hereditary bowel cancer?
The following may help you and your GP assess your personal level of risk.
High bowel cancer risk
Hereditary conditions
- Relatives diagnosed with Familial Adenomatous Polyposis (FAP)
- Relatives diagnosed with Lynch syndrome (HNPCC)
- Siblings of people with MYH-associated polyposis (an autosomal recessive condition)
- Three or more first-degree relatives diagnosed with bowel cancer at any age; or
- Two first-degree relatives AND two or more second-degree relatives diagnosed with bowel cancer at any age; or
- Two first-degree relatives AND one second-degree relative diagnosed with bowel cancer, with at least one diagnosed before age 50.
Please note: a first-degree relative can be a parent, brother, sister or child.
A second-degree relative can be an aunt, uncle, grandparent, grandchild, niece, nephew, or half-brother or half-sister.
- One first-degree relative diagnosed with bowel cancer before age 60 years; or
- One first-degree relative AND one or more second-degree relatives diagnosed with bowel cancer at any age; or
- Two first-degree relatives diagnosed with bowel cancer at any age.
Personal health history
- Bowel cancer
- Special types of polyps, called adenomas
- Inflammatory bowel disease such as ulcerative colitis or Crohn's disease
Near average bowel cancer risk
- One first-degree relative diagnosed with bowel cancer at 60 years or older.
Average bowel cancer risk
- Age 40 or over; and
- No symptoms to suggest bowel cancer; and
- No first-degree or second-degree relative diagnosed with bowel cancer.
The three most common inherited syndromes linked with bowel cancers are:
- Hereditary Non-Polyposis Colorectal Cancer (HNPCC) (also known as Lynch Syndrome)
- Familial adenomatous polyposis (FAP)
- MYH-Associated Polyposis (MAP)
In HNPCC, mutation carriers' lifetime risk for bowel or other syndrome cancers is 70-90%.
If a person has a HNPCC mutation, each of their children has a 50% chance of inheriting the mutation.
Lynch syndrome is caused by a change in a gene that normally functions to protect a person from getting cancer.
Each person inherits genes from both their parents and HNPCC is caused by a fault in one of the genes known as the 'mismatch repair' genes.
Someone who inherits HNPCC from their parents has a normal gene and a 'faulty' gene, which increases their risk of developing bowel cancer and other types of cancer.
HNPCC affects less than 5% of those who develop bowel cancer. Although rare, this risk relates to a clear family history of bowel or specific, related cancers e.g. some gynaecological cancers, digestive tract, urinary tract, brain or bowel cancer.
The typical age of diagnosis of this kind of Hereditary Non-Polyposis Colon Cancer (HNPCC or Lynch Syndrome) is usually between 40-50 years (compared to 60-70 years amongst the general population).
In families where there is a clear history of HNPCC, screening with colonoscopy every 1 to 2 years usually commences from age 25 or 5 years earlier than the youngest affected family member if they were diagnosed under 30, whichever comes first.
Where HNPCC is suspected, your GP will refer you to a Family Cancer Clinic for support and on-going management of the condition.
| Familial Adenomatous Polyposis (FAP)
An affected person has a 50% chance of passing the condition on to each of their children.
FAP is characterised by the presence of hundreds to thousands of adenomatous polyps in the large bowel of affected individuals, which often start in adolescence.
Cancerous polyps are very common in this condition, usually by age 40, without active management of the polyps and screening on a regular basis.
Diagnosis is usually made following colonoscopy to confirm the presence of polyposis. Testing for mutation of the APC gene currently detects 95% of mutations present.
In families where there is a clear history of FAP, annual screening via a flexible sigmoidoscopy or colonoscopy usually commences from age of 10-15 or earlier if there are gastrointestinal symptoms.
Where FAP is suspected, your GP will refer you to a Family Cancer Clinic for support and on-going management of the condition, because it has been known to affect adolescents and teenagers.
The treatment for FAP is usually a planned operation to remove the affected part of the colon once polyposis has become established. This normally occurs in the late teens or early twenties.
These are very rare conditions and you will need the specialist help and support of an experienced colorectal team to help make the right decisions for the individual affected.
Although considered rare, people diagnosed with MYH-Associated Polyposis (MAP) have close to 100% risk of developing bowel cancer by the age of 65, if they are not monitored closely with colonoscopy.
MAP is characterised by the development of 10 to a few hundred polyps, which can develop into cancer.
A person has a 25% chance of being affected with MAP when both parents pass on the gene mutation.
MAP is a genetic condition caused by a mutation in the MYH gene, also known as the MUTYH gene.
In order for a person to have an increased risk of MAP, each parent must pass on a copy of the altered MUTYH gene.
A person who has only one copy of the gene mutation (from one parent) is called a carrier, and they are not at increased risk themselves. However they may pass the gene on to their children.
Most individuals with MAP will develop dozens, sometimes hundreds, of polyps, in their colon over their lifetime. It is rare that people with MAP will have no polyps present at all.
The risk of bowel cancer is increased if these polyps are not removed.
In families where there is a history of MAP, your GP will refer you to a Family Cancer Clinic for support and ongoing management of the condition.
Where MAP is suspected, individuals and families should undergo DNA testing, and test for MAP in those who do not have a mutation in the APC gene (APC gene associated with FAP/AFAP).
Do you know if anyone in your family has had bowel or any other kind of cancer? Talk to your family and make sure you all know your family history.
If you think that you have a strong family history of bowel cancer, you should make an appointment with your GP to talk about your concerns.
If your GP agrees with you, they will refer you to a Family Cancer Clinic.
A genetic specialist will go through your family history with you in great detail and ask you to provide accurate information about who has been affected, how old they were when they were diagnosed, and the site where their cancer developed.
You may also have to have blood tests as part of this investigation.
If the genetic specialist agrees you are at increased risk, you will be referred to a specialist to talk about what types of screening and/or surveillance they recommend, at what age you (and/or other family members) should commence screening and/or surveillance and how often.
Regular screening and/or surveillance will ensure that any signs of bowel cancer are detected and treated early.
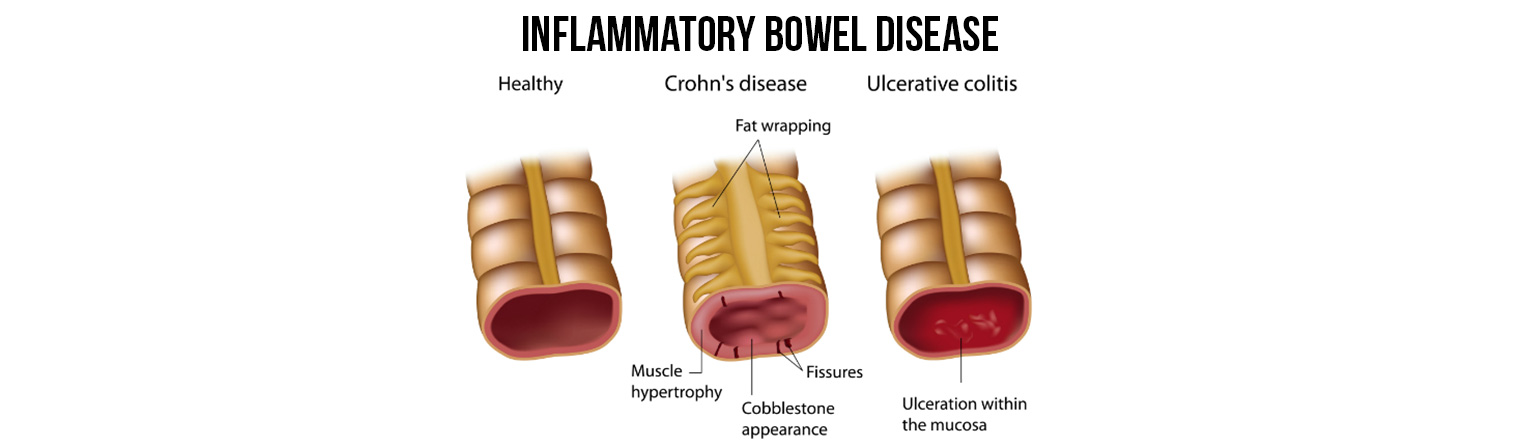
Inflammatory bowel disease is sometimes shortened to IBD. However, this is not the same as IBS, which is short for irritable bowel syndrome, and which is a very different condition.
Both these conditions can cause inflammation of the colon and rectum, with similar symptoms and treatments.
The main differences are that the inflammation of ulcerative colitis is usually found just in the inner lining of the gut, while in Crohn's disease the inflammation can spread through the whole wall of the gut.
In addition, ulcerative colitis only affects the colon and rectum, while Crohn's disease can affect any part of the gut.
Crohn's disease is a long-term condition that causes inflammation in the gut – the lining of the digestive system.
The inflammation usually occurs in the last section of the small intestine (ileum) or the large intestine (colon), but any part of the gut can be affected.
There may be a small patch of inflammation, or it may spread quite a way along the gut, or there may be several patches in different places.
In a few people, the mouth, gullet or stomach may be involved. More rarely, the condition also triggers inflammation outside the intestine leading to arthritis, eye inflammation or skin complaints.
In mild Crohn's disease, there are patches of inflammation with groups of small ulcers, similar to mouth ulcers.
In moderate or severe Crohn's disease, the ulcers are larger and deeper. The inflammation can thicken the intestine, blocking the passage of digested food.
In some cases, deep ulcers break through the intestine wall causing infection – an abscess – outside the bowel. This infection or abscess can spread to a nearby part of the body, often around the anus, and this is called a fistula.
Scar tissue can form as the inflammation heals, and in some cases this leads to a blockage in the intestine.
Who gets Crohn's disease?
Crohn's disease is a rare condition. It can develop at any age, but usually starts between the ages of 15 and 30, and between the ages of 60 and 80.
Crohn's disease affects slightly more women than men.
The condition runs in families, so those who have a family member with Crohn's disease are more likely to develop the condition too.
It is also more common in people who have had their appendix removed, for the first five years after the operation.
What causes Crohn's disease?
The exact cause is unknown. Most researchers think that it is caused by a combination of factors.
These include:
- Genetics
Inherited genes may increase the risk of developing Crohn's disease. - Immune system
One theory is that the immune system – the body's natural defence against infection and illness – is responsible for the inflammation in the digestive system. Crohn's disease disrupts the immune system, so that it no longer recognises the 'friendly bacteria' that help to digest food. - Previous infection
A previous infection, possibly in childhood, may trigger an abnormal response from the immune system. - Environmental factors
Crohn's disease is most common in countries with a modern western lifestyle, such as Australia, and least common in poorer parts of the world, such as Africa. This suggests that the environment has a part to play. - Smoking
Smokers are twice as likely to develop the disease compared with non-smokers. Smokers with Crohn's disease usually have more severe symptoms than non-smokers.
What are the symptoms?
The symptoms vary and depend on which part of the intestine is inflamed.
There may be long periods that last for weeks or months with very mild or no symptoms, known as remission.
This may be followed by periods when the symptoms are particularly troublesome, known as flare-ups.
Common symptoms include one or more of the following:
- recurring diarrhoea, often with a feeling of urgency to get to the toilet, and often with a feeling of wanting to go to the toilet but with nothing to pass
- abdominal pain and cramping, which is usually worse after eating
- extreme tiredness (fatigue)
- weight loss
Less common symptoms include:
- high temperature (fever) of 38°C or above
- feeling sick (nausea)
- being sick (vomiting)
- joint pain and swelling (arthritis)
- inflammation and irritation of the eyes
- skin rashes
- blood and mucus in poo, which may be the result of an ulcer bleeding
- anaemia, which may occur if there is a lot of blood loss
- mouth ulcers
If your GP suspects that the symptoms might point to Crohn's disease, a referral will be made to a specialist for diagnostic tests.
Is there a link between Crohn's disease and bowel cancer?
People with Crohn's disease have an increased risk of developing bowel cancer and should be monitored regularly.
The risk is related to the length of time that inflammation has been present, and the site and severity of the disease.
Several studies estimate the risk by following patients over a period of 10–40 years.
Some did not show an associated risk, but others predicted an increase that was twice that of the general population for developing bowel cancer.
If the disease is confined to the colon, this risk is estimated at around five times greater.
The risk of small intestinal cancer has been estimated at around six times that of the general population, but as this is an extremely rare cancer in the general population, the risk in Crohn's disease is still small.
While Crohn's disease and bowel cancer are two very different conditions, it is important to note that many of the symptoms are the same for both.
The signs and symptoms may vary according to the site and extent of the cancer, but mostly show a general worsening of the symptoms associated with Crohn's disease.
People with Crohn's disease are often unaware that they have bowel cancer, as the initial symptoms are similar to Crohn's disease, such as blood in your poo, diarrhoea and abdominal pain.
Because of this, you will probably be advised to have a colonoscopy every few years to check that no cancer has developed.
Ulcerative colitis is a long-term, chronic condition that usually occurs in the rectum (the part of the large bowel that lies just inside the anus) and lower part of the colon, but it may affect the entire colon (large intestine).
The colon becomes inflamed and, if this inflammation becomes severe, the lining of the colon is breached and ulcers may form.
The amount of inflammation in ulcerative colitis is very variable, and many people never develop ulcers, because their degree of inflammation is not that advanced.
In mild cases, the colon can look almost normal, but when the inflammation is widespread, the bowel can look very diseased and can contain ulcers.
Who gets ulcerative colitis?
The exact cause is unknown. Most researchers think that it is caused by a combination of factors. These include:
- Genetics
Inherited genes may increase the risk of developing ulcerative colitis.
- Immune system
Ulcerative colitis is called an autoimmune condition. This means the immune system – the body's natural defence against infection and illness – goes wrong in some way and attacks healthy tissue. One theory is that the immune system mistakes the harmless bacteria – the 'friendly bacteria' inside the colon that help to digest food – as a threat and attacks the tissues of the colon, causing it to become inflamed. - Environmental factors
Ulcerative colitis is most common in countries with a modern western lifestyle, such as Australia. This suggests that the environment has a part to play, and various factors have been suggested. These include air pollution; diet; and hygiene (the result of children being brought up in increasingly germ-free environments).
What are the symptoms?
The symptoms vary, and range from mild to severe. It depends on how much of your colon is affected and the level of inflammation.
Symptoms are often worse first thing in the morning. Symptoms can flare up and then disappear, known as remission, for months or even years. This may be followed by periods when the symptoms are particularly troublesome, known as flare-ups.
Common symptoms include one or more of the following:
- diarrhoea, with or without blood and mucus
- abdominal pain
- a frequent need to go to the toilet
- weight loss
Other symptoms include:
- tiredness (fatigue)
- loss of appetite
- weight loss
- anaemia (shortness of breath, irregular heartbeat, tiredness and pale skin)
- high temperature (fever) of 38°C or above
- dehydration
- a constant desire to empty the bowels
- bloating and gas
- heartburn and reflux
How is ulcerative colitis diagnosed?
The starting point during an initial assessment is for your GP to ask about the pattern of symptoms, your general health and medical history, and whether there is a family history of ulcerative colitis.
An examination will look for signs of inflammation, such as tenderness in the abdomen, and paleness that might be caused by anaemia.
If your GP suspects that the symptoms might point to ulcerative colitis, a referral will be made to a specialist for diagnostic tests.
Tests to diagnose ulcerative colitis may include one or more of the following:
- blood test, to check for inflammation, anaemia and protein levels
- stool sample, which is checked for infection
- X-rays, to help assess the extent of the condition
- sigmoidoscopy, to examine the extent of inflammation in the rectum and lower part of the colon
- colonoscopy, to examine the inside of the entire colon
- how many times you are passing stools
- whether those stools are bloody
- whether you also have more wide-ranging symptoms such as fever, rapid heartbeat and anaemia
- how much control you have over your bladder
- your general well-being
What treatments are available?
There is currently no cure for ulcerative colitis. However, medication can improve symptoms and surgery can also help in many cases.
People with ulcerative colitis have an increased risk of developing bowel cancer and should be monitored regularly, especially if the condition is severe or extensive.
The longer you have ulcerative colitis, the greater the risk is:
- after 10 years the risk of developing bowel cancer is 1 in 50
- after 20 years the risk of developing bowel cancer is 1 in 12
- after 30 years the risk of developing bowel cancer is 1 in 6
People with ulcerative colitis are often unaware that they have bowel cancer as the initial symptoms are similar to ulcerative colitis, such as blood in your poo, diarrhoea and abdominal pain. Because of this, you will probably be advised to have a colonoscopy every few years to check that no cancer has developed.