| Life after treatment
Many people diagnosed with bowel cancer will undergo successful treatment, and life can soon get back to normal.
Keeping positive during treatment, and asking for support when you need it, can help you get through the traumatic experience of having cancer.
You will be regularly tested to check that the cancer has not returned. If after five years, it has not returned, you are considered clear and it's time to celebrate!
Do ask for this help when you are first admitted to hospital so that proper arrangements can be made.
- Take your painkillers regularly, as prescribed, until you no longer have pain or discomfort. You may need to do this for some weeks after surgery to help you move about comfortably.
- Get out of bed and get dressed every day, helping to build up your strength.
- Gradually start to increase your activity by doing some light jobs around the house.
- Tell friends and family that it will take some time (at least six weeks) before you are back to your normal self and able to undertake all your usual activities.
- Start doing some form of gentle exercise as soon as you can, several times a day. Start with a short walk (10 minutes) and increase the distance as you feel able. By about six weeks you should be able to walk for half an hour or more.
- Avoid lifting any heavy items and doing heavy household chores for at least six to ten weeks, thereby reducing the risk of developing a hernia or other complications.
- Drink plenty of fluids and eat light, nutritious meals frequently throughout the day.
Diarrhoea, increased frequency or urgency of bowel motions can also be common problems after bowel surgery. Again, your GP can prescribe medication to help with this.
If you have one large wound, following emergency surgery or if a laparoscopic procedure resulted in open surgery, this can result in a longer hospital stay. After keyhole surgery you may have two or three small wounds, which heal more quickly.
If you have a large wound, your stitches or staples will be able to be removed around ten days after surgery.
- a high temperature
- unable to eat or drink for any reason
- persistent diarrhoea, nausea or vomiting
- constipation for three days or more
- pain, swelling, redness or unexpected leakage around your wound or stoma
Psychological issues
The information below describes exercises which may help you regain control. There are also some medicines which may help, if necessary.
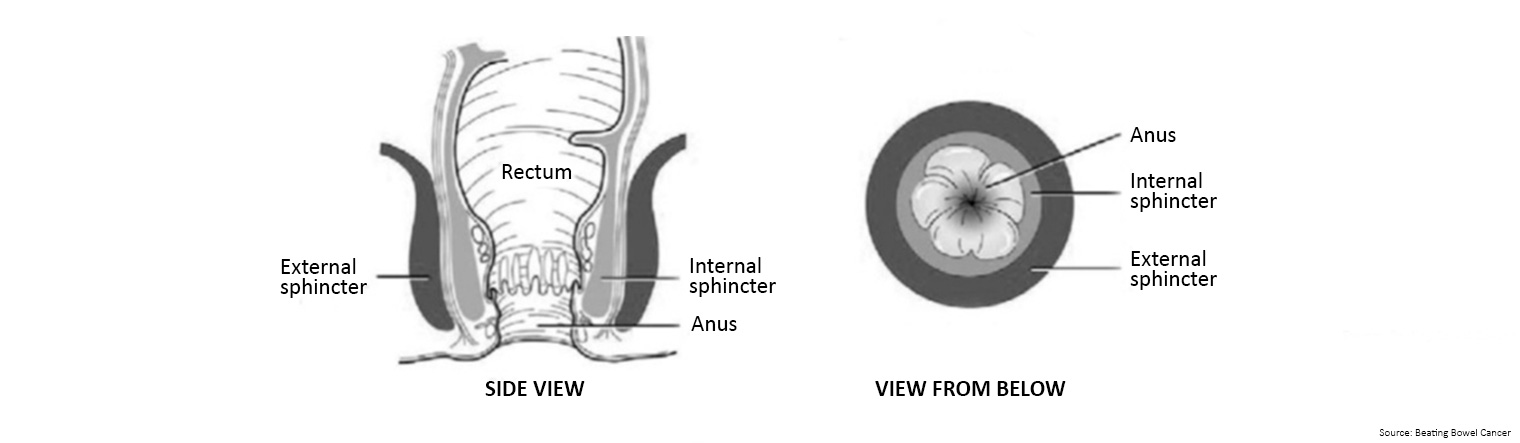
Sensitive nerve endings in the anus can tell you if it is gas or poo waiting to come out. If it is poo, you squeeze the second muscle to stop it from coming straight out.
The squeezing moves the poo back into the rectum, where it waits until you get to the toilet. You may not be able to squeeze enough to hang on if your muscles are weak or have been damaged by surgery, or they do not squeeze in the correct order or the nerve supply to the muscles is damaged.
There are many different reasons why you might develop bowel leakage or incontinence following treatment for bowel cancer. For example, surgery which involves removing part of the bowel, shortening it or changing its shape, will affect its normal working pattern.
It can also change how sensitive the nerve endings around the bowel area are, or in rare cases, cause damage to the anus – the sphincter muscle which forms the entry into your rectum (back passage).
Chemotherapy treatments can also cause side effects in the bowel, and these can take some time to settle down again. In a few cases, radiotherapy treatments can also cause short term and longer term changes to the way you are used to your bowel working.
Whatever the reason, having a problem controlling your bowels can be upsetting. If you have had the distressing experience of a bowel accident in public, you will be acutely aware of the feeling of any pressure or filling sensation in your rectum which might mean you will need to find a toilet quickly. It is a natural reaction to try and prevent an accident by either tensing all your muscles and holding your breath or rushing to find a toilet. A better course of action is to sit or stand still, breathe deeply and contract your anal sphincter until the urge passes.
Your rectum, your sphincter muscles and your confidence need retraining to help you overcome this problem.
Exercises can strengthen these muscles so that they give support again. This will improve your bowel control and improve or stop leakage of gas or poo. Like any other muscles in the body, the more you use and exercise them, the stronger they will be.
Imagine that your sphincter muscle is a lift. When you squeeze as tightly as you can, your lift goes up to the fourth floor. But you cannot hold it there for very long, and it will not get you safely to the toilet as the muscle will get tired very quickly. So now squeeze more gently and take your lift only up to the second floor. Feel how much longer you can hold it than at the maximum squeeze.
You may not be able to do this at first. If the urge is too strong, start by trying to delay bowel emptying once you are sitting on the toilet. See how long you can wait until you really have to let go.
Sit on the toilet and hold on for as long as you can before opening your bowels. If you can only manage a few seconds, don't worry, it will become easier with practice. You might find it easier if you try to relax and concentrate on breathing very calmly. It may be helpful to take something to read.
Once you are able to delay opening your bowels for a few minutes, the unpleasant urge to go then disappears. Get up and leave the toilet. Return a few minutes later when there is no urge and try to open your bowels.
Gradually you will find that you can increase the distance and time away from the toilet. The more you practise this and the sphincter exercises below, the sooner it will happen.
Eventually you should find that you are regaining control of your bowels. The longer you can hold on, the more fluid is absorbed from the poo and so the firmer and less urgent they become.
When you have some successes, you will become more confident. The less you panic, the easier it is to make the urge go away.
- Sit, stand or lie with your knees slightly apart. Now imagine that you are trying to stop yourself passing wind from your bowel. To do this you must squeeze the muscle around your back passage. Try squeezing and lifting that muscle as tightly as you can, as if you are really worried that you are about to leak. You should be able to feel the muscle move. Your buttocks, tummy and legs should not move much at all. You should be aware of the skin around your back passage tightening and being pulled up and away from your chair. You should not need to hold your breath when you tighten these muscles.
- Tighten and pull up the sphincter muscles as tightly as you can. Hold for at least five seconds and then relax for at least 10 seconds. Repeat at least five times. This will work on the strength of your muscles.
- Pull the muscles up to about half of their maximum squeeze. See how long you can hold this. Then relax for at least 10 seconds. Repeat at least five times. This will work on the endurance or staying power of your muscles.
- Pull up the muscles as quickly and tightly as you can, then relax, and then pull up again. See how many times you can do this before you get tired. Try for at least five quick pull-ups. Do these exercises at least 10 times every day. As the muscles get stronger, you will find that you can hold for longer than five seconds, and that you can do more pull-ups each time without the muscles getting tired. Remember that you cannot hold your tightest squeeze for very long, so it is better to use a gentle squeeze that you can hold for longer. Your control will gradually improve. You may need to exercise regularly for several months before the muscles gain their full strength and continue to exercise to maintain your bowel control.
There are some foods and medicines that can affect how loose or firm your poos are and it may take a bit of time to work out which ones might be adding to or helping the problem.
- 5FU (FOLFOX)
- capecitabine (XELOX or CaPOX)
- 5FU and irinotecan (FOLFOXFIRI)
They are often triggered by eating, drinking, or touching something cold or breathing cold air. Most people cope well with the short-term symptoms of peripheral neuropathy with only a few changes to their lifestyle.
Symptoms include:
A change in sensation
You may have a feeling of heaviness, burning or pins and needles in the affected area. Or, you may notice unusual sensations, such as a feeling of warmth or burning when touching something cold. Or, you may notice a loss of sensitivity or feeling, starting in your feet and fingertips.
Increased sensitivity and pain
For the first 48 hours after your treatment, you will feel much more sensitive to the cold. You may find that even light touch or pressure in the affected area feels uncomfortable or painful. You may experience a sharp or burning sensation, or it may feel like minor electric shocks. You may also feel a tingling in your face or tongue. If the pain becomes more severe, your specialist can prescribe medication to help relieve it.
Difficulty with balance, walking and coordination
If your feet and/or lower legs are affected, this may make it difficult to walk, climb stairs or keep your balance. You may find that you stumble or trip more often, especially on uneven surfaces.
Difficulty with everyday tasks
You may feel clumsy at times and less in control of your movements. If your fingers are affected, you may not be able to do ‘fiddly’ tasks, such as fastening buttons or tying your shoelaces.
- It is important to protect your hands and feet by keeping them warm at all times.
- Use gloves when you go out in cold weather and to avoid touching anything cold.
- Wear socks to keep your feet warm. Don’t walk around barefoot at home.
- Cover your mouth with a scarf or face mask to filter cold air.
- Don’t eat or drink cold or even cool foods. Eat food that is at room temperature.
- Don’t sit in an air-conditioned room or car.
- Try to go for a walk every day, even for a short distance. This will prevent muscle weakness, which adds to your general lack of balance. Wear soft shoes and add padded insoles to make walking less painful.
- Do not wear tight fitting socks or shoes. Ensure your socks are natural fibres to allow your skin to breathe.
- Always test water with part of your body not affected by neuropathy, such as your elbow, before you bathe, shower, or wash dishes. Turn your hot-water thermostat to a lower setting. It is easy to burn yourself if you cannot judge the temperature of water.
- Always wear gloves when working in the garden and use oven gloves in the kitchen to avoid injury. Take special care with kitchen knives and tools.
- Clear your house and garden of things you might trip on such as rugs, slippery surfaces and clutter on stairs and steps. Make sure rooms are well lit and always put a light on if you get up during the night.
- Put a skid-proof mat in the bathtub or shower, and consider using a shower stool.
- If you have problems balancing or walking, ask for a referral to a physical therapist to strengthen muscles, build balance, or prescribe a walking aid. An occupational therapist may be able to help adapt your home so daily activities are easier and safer for you.
- Check your feet every day for redness, injuries, or blisters and tell your specialist or nurse if you are concerned. It is important to avoid an infection developing.
Keep track of tingling, pins and needles, numbness, pain, or difficulty with normal activities and let your specialist know if they are getting worse. It is possible to reduce the dose or to change your treatment regime so that oxaliplatin is given less frequently.
There are many treatments that can be tried to ease the discomfort and its effect on your life such as physical therapy, relaxation therapy, guided imagery, and acupuncture. If your symptoms don’t improve you may need to be referred to a pain clinic.
If your specialist thinks that you may be lacking in minerals, due to your diet, the amount of alcohol you drink or for some other reason, you may be given an infusion of calcium or magnesium to help reduce the symptoms.
If the oxaliplatin is stopped because of worsening symptoms, you will continue to receive the capecitabine or 5FU which is given with it. However, if your symptoms continue to get worse, your specialist may suggest that you try another type of anticancer drug or decide to give you a break from chemotherapy.