- Neo-adjuvant (pre-operative) radiation therapy: is used to shrink rectal cancer tumours, making it easier to surgically remove them and reducing the risk of the cancer returning. When radiotherapy is given at the same time as a small dose of chemotherapy it is called chemo-radiotherapy.
Chemo-radiotherapy can also be used on its own to kill cancer cells as an alternative to chemotherapy and/or surgery and is usually the first treatment offered to patients with anal cancer
Whether you have external or internal radiotherapy, there will be a period of time between the radiotherapy treatment ending and your surgery. This delay is intentional, as the radiotherapy continues to shrink the tumour for several weeks after the end of treatment.
- Adjuvant (post-operative) radiation therapy: may be recommended if you did not receive radiotherapy before your surgery, in order to destroy any cancer cells that were left behind. This could result if a tumour was difficult to remove or grew through the wall of the rectum or spread to nearby lymph nodes.
- Palliative radiation therapy: involves giving lower doses of radiotherapy over a shorter period of time. It can also be given when surgery is not an option, to relieve symptoms or slow the spread of the cancer.
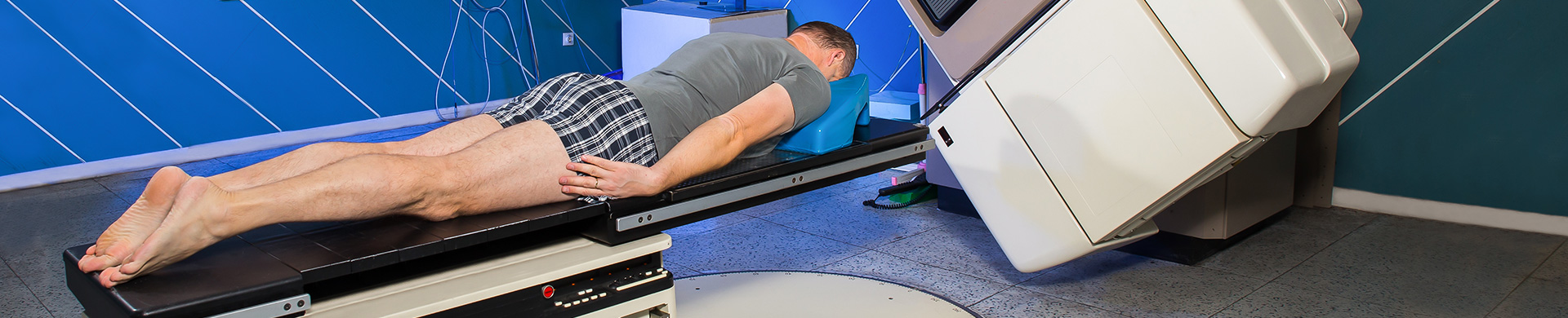
- External radiation therapy: is delivered from outside of the body by a machine and only takes a few minutes, although the planning session takes longer. It is usually given as a course of several treatments over days or weeks. Each time you are given radiotherapy you receive a ‘fraction’ of the full dose prescribed.
- Internal radiation therapy: also known as brachytherapy or contact radiotherapy, involves positioning radioactive sources near to or inside the tumour. This treatment delivers a high dose of radiation directly to the cancer while limiting damage to surrounding tissues and organs.
- Intensity modulated radiotherapy (IMRT): is radiation therapy where both the radiotherapy beam and the dose within the beam are shaped to match the tumour’s shape and thickness. IMRT gives less radiotherapy to normal tissues compared to standard radiotherapy and research is starting to show that it causes less severe side-effects.
Specialists are now also looking at a new type of IMRT called volumetric modulated arc radiotherapy (VMAT). This is where the radiotherapy machine rotates around the body, continuously reshaping and changing the intensity of the radiotherapy beam.

Radiation therapy can destroy cancer cells, but it can also have an effect on some of the surrounding normal cells.
Side effects depend mainly on the amount of radiation given and the part of your body that is treated.
You are likely to become very tired during radiation therapy, especially in the later weeks of treatment. Resting is important, but specialists usually advise patients to try to stay as active as they can. Many patients find they can still continue to work during the radiation period, usually with some adjustment of work hours. However, towards the end of radiotherapy, the majority of patients will need to take significant time off work (often the last two weeks of chemo-radiotherapy and the two weeks following).
- Why do I need this treatment?
- When will the treatments begin?
- When will they end?
- How will I feel during treatment?
- How will we know if the radiation treatment is working?
- What can I do to take care of myself during treatment?
- Can I continue my normal activities?
- Are there any lasting effects?
Bowel irritation
If you don’t have a stoma you may notice you go to the toilet more frequently, pass a lot of wind, have a feeling of urgency or develop discomfort when passing a motion. Some people may also develop rectal bleeding or a mucous discharge. Occasionally people may complain of stomach cramps. Changing your diet may help.
The skin around the pelvis may be affected by radiotherapy. After a few weeks of treatment, this area may become pink in colour and the skin around the anus may also become sore and red – similar to sunburn. Any irritation is generally relieved by sorbolene cream. It is also possible to lose some pubic hair, however this is usually temporary. If this type of reaction worsens, your doctor may prescribe a steroid cream. Regular sitz baths (1 tablespoon of salt in a cool shallow bath) may also relieve any discomfort or pain.
During treatment, your hip joints will receive some radiation. In some cases this can cause the bones in your pelvis/hips to become weak. This may also increase the risk of fracture. Modern equipment and planning techniques ensure the radiation dose to the hip and sacrum areas is kept at low levels, so that the risk of fracture is minimised.
Sexual function - men
For men who have had surgery for rectal cancer, there is always a risk some of the nerves responsible for having an erection can be damaged. These problems may not become evident until years after treatment. Sterility is another potential risk from having this treatment. Treatment techniques can be altered and options are available so please talk to your doctor if you are concerned.
Your diet
Maintaining an adequate and highly nutritious diet is crucial during treatment, as well as afterwards because cancer, and its treatment, place extra demands on the body. However, this can sometimes be very difficult towards the end of the treatment phase.
Speak with a nutritionist or dietitian early during your treatment phase to address potential nutritional issues. They can help you with all aspects of improving the way you eat. Contact Bowel Cancer Australia’s Bowel Care Nutritionist for additional advice and support.
It involves injecting very small radioactive particles known as SIR-Spheres into the blood supply of the liver. Because of their size, the microspheres lodge in the small blood vessels of the tumours where they deliver a localised dose of radiation.
SIRT provides an opportunity to irradiate cancer inside the liver that cannot otherwise be treated by surgery or other techniques. SIRT also minimises radiation damage to healthy cells in other parts of the body.
There is some evidence that SIRT can help slow the progression of the disease in combination with chemotherapy.
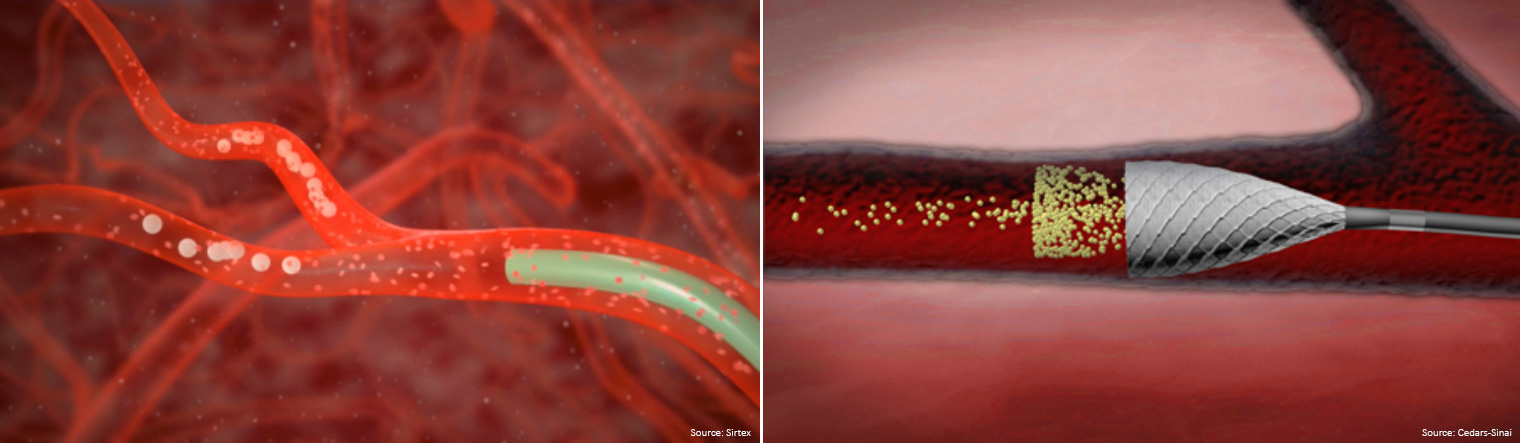
They are extremely small resin beads that contain the radioactive substance yttrium-90 (Y-90).
Due to the unique anatomy of the liver and its blood supply, these microspheres can be delivered directly into any liver tumour.
At about one-third the diameter of a strand of hair, the microspheres are small enough to travel through the hepatic arteries, but too large to pass through the smallest blood vessels in the tumour where they become lodged. The radiation emitted from the microspheres extends about 1cm into surrounding tissues and lasts from 2-4 weeks. This targeted treatment allows maximum radiation to be administered to the tumour cells while reducing exposure to the remaining healthy tissue.
When is SIRT a treatment option?
SIRT is used where cancer in the liver cannot be removed with surgery or techniques such as radiofrequency ablation.
- SIRT is only suitable for bowel cancer patients where the liver is the only or main site of disease. SIRT has no effect on cancer outside the liver.
- Patients must have a sufficiently healthy liver, which can usually be determined by a simple blood test.
- Radiation therapy is not suitable for women who are pregnant or breast-feeding or intend to become pregnant or breastfeed within two months of treatment. Radiation may cause irreversible harm to an unborn baby or infant.
Preparation for SIRT
Your treatment team, that will include a specialist known as an interventional radiologist, will ask about your previous cancer history and other medical conditions.
They will conduct initial tests to ensure that it is possible for you to receive SIRT safely. SIRT involves two procedures performed under conscious sedation. Both procedures will include a radiology procedure known as an angiogram.
The purpose of the first procedure is to map and prepare your liver for SIRT. During the mapping procedure your interventional radiologist will block some blood vessels to minimize the potential for the microspheres to travel beyond your liver (e.g. to the stomach or intestine). You will also receive a small amount of radioactive 'test beads' to check for any flow of beads from the liver to the lungs.
Assuming that the results of these initial tests are acceptable, the appropriate dose of SIR-Spheres microspheres will be determined. The SIR-Spheres microspheres will then be administered during a second procedure, which is typically conducted one to two weeks after the initial tests are completed.
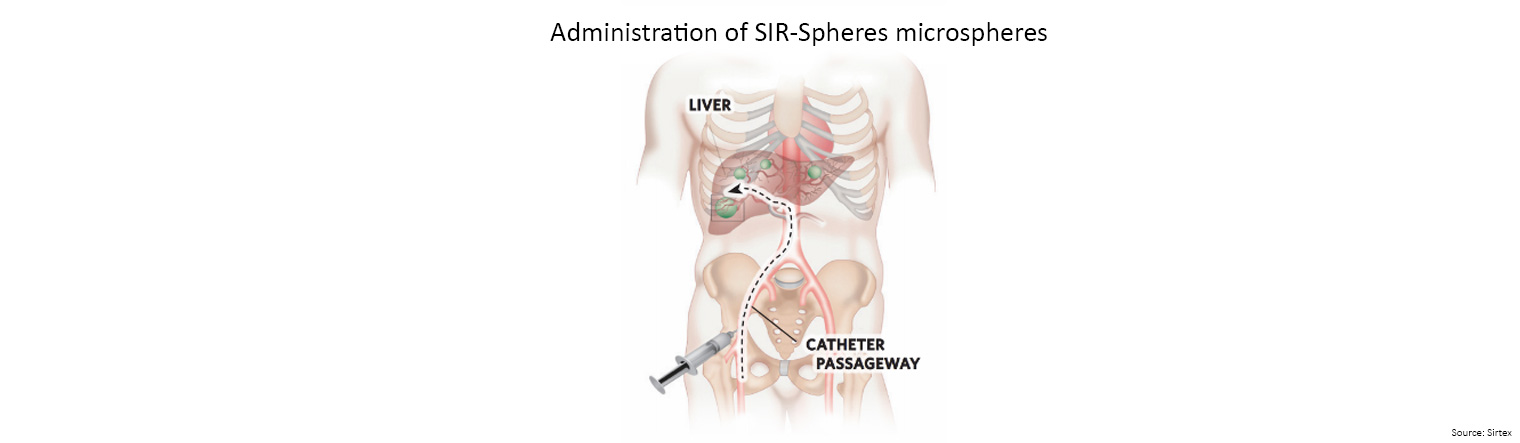
A small flexible tube, known as a catheter, is then guided through the artery into the liver.
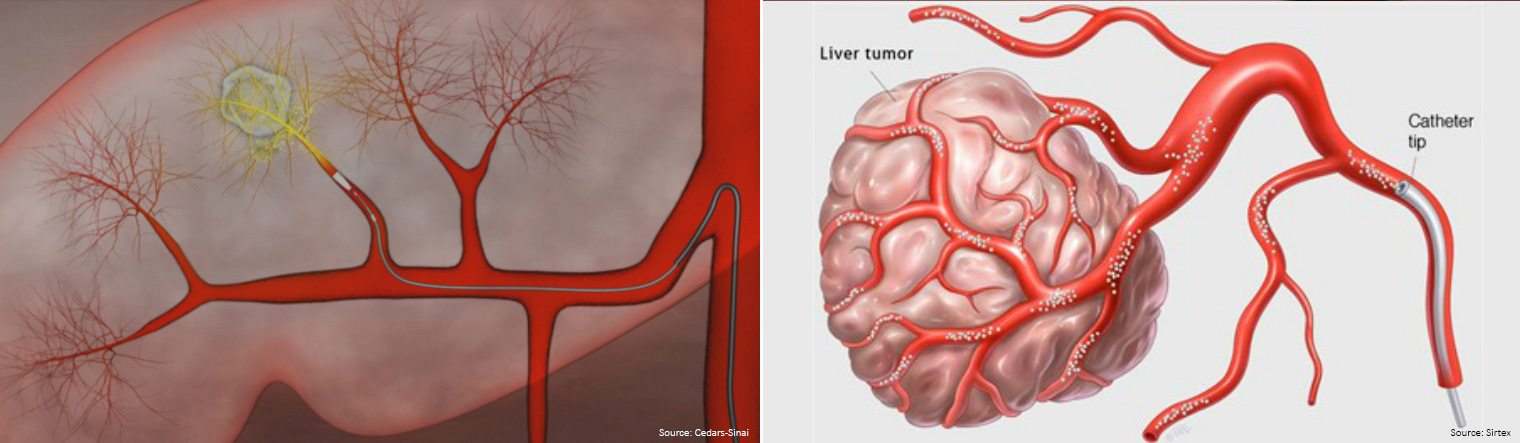
The SIR-Spheres microspheres are administered through this catheter.
You will also be monitored for a few hours after the procedure to enable the treatment team to determine whether you have any side effects or complications that require additional medication.
Since you will have received a radioactive treatment, there are some simple precautions that need to be taken during the first 24 hours following SIRT procedure.
- thorough washing of your hands after going to the toilet
- cleaning up any spills of body fluids such as blood, urine, or stools and disposing of them in the toilet
Your treatment team will provide you with further information on these precautions. Your treatment team will also monitor your progress using blood tests and radiography scans at periodic intervals.
Your oncologist will determine if your chemotherapy needs to be stopped during this time. Most patients stop two weeks before SIRT and for two weeks after.
How soon can I go home after SIRT?
Normally, you can be discharged 4-6 hours after the procedure. Most patients can resume their normal daily activities within two to three days. In rare cases, some patients may need to stay overnight in the hospital for observation.
What are possible side effects of SIRT?
Many patients experience abdominal pain and nausea, which normally subside after a short time or with routine medication. Many patients also develop a mild fever that may last for up to a week and fatigue, which may last for several weeks. Pain-killers, anti-inflammatory, anti-nausea and anti-ulcer drugs can help prevent or minimise these side effects.
Are there any serious complications associated with SIRT?
In rare instances and even in experienced hands, there is the possibility that some microspheres may inadvertently reach other organs such as the gall bladder, stomach, intestine or pancreas where they may cause inflammation. Your treatment team will have received special training to minimise or manage these risks.
Will I lose my hair?
Hair loss has never been reported following treatment with SIR-Spheres microspheres. If you are receiving chemotherapy this may cause hair loss, however SIR-Spheres microspheres will not make this worse.
Will I have to change what I eat or drink?
You should continue to eat and drink as normal. Adequate levels of food and in particular, fluids, will help you return to your normal daily activities. Your specialist is the best person to advise you regarding alcohol consumption.