What are patient-reported measures? | What are PREMs? | What are PROMs? | A global standard in bowel cancer patient care | The ICHOM Working Group
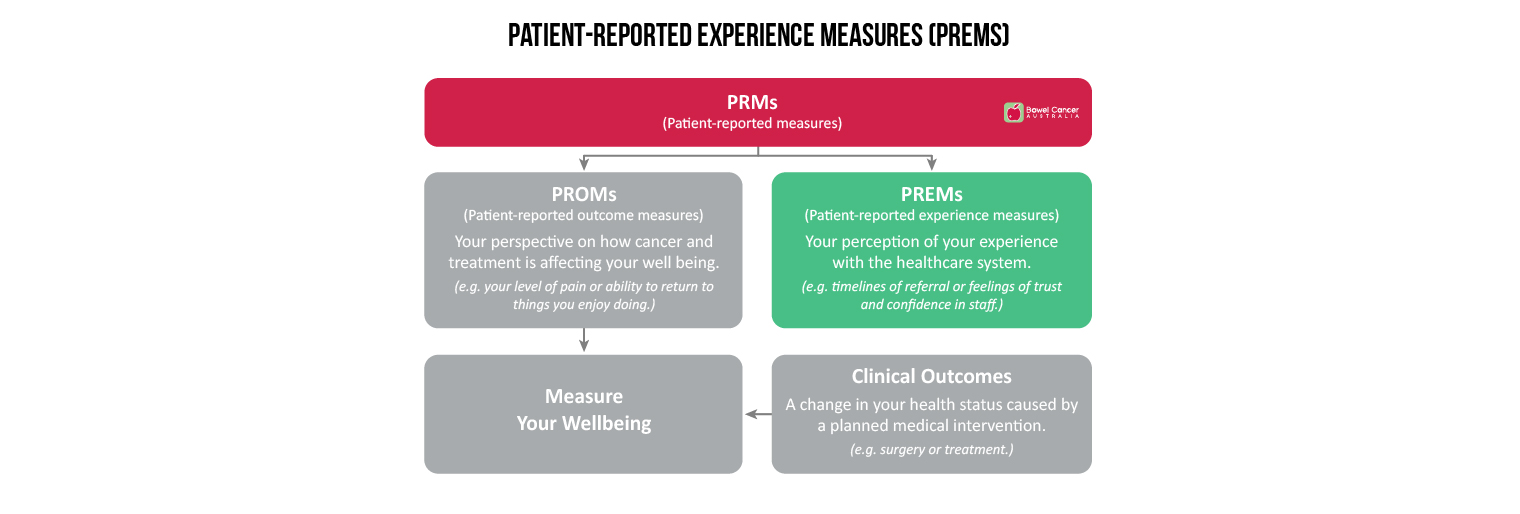
Patient Reported Measures (PRMs) are questionnaires that capture a patient’s perspective of their health, healthcare experiences and the impact disease and treatment is having on their wellbeing.
There are two types of PRMs -
- Patient-Reported Experience Measures (PREMs) ask patients about their healthcare experience.
- Patient-Reported Outcome Measures (PROMs) ask patients about how cancer, treatment, and side-effects are affecting their life.
| What are patient-reported experience measures (PREMs)?
Patient-reported experience measures (PREMs) are questionnaires that capture a patient’s perspective on health service delivery (e.g., communication with nurses and doctors, staff responsiveness, discharge, and care coordination) and can be used as important and meaningful measures of quality of care to drive improvement and monitor performance.
By asking patients questions about their experience using a PREMs questionnaire, it is possible to find out what processes are working well and identify areas for improvement, so that hospitals and healthcare services can address them.
Bowel Cancer Australia’s My Colonoscopy Experience is a PREMs questionnaire.
It allows you to report what the colonoscopy experience was like for you, because as a patient you can see signs of high or poor quality that may not be seen by staff.
With 1.1 million colonoscopies to be performed in Australia by 2021, the My Colonoscopy Experience questionnaire remains open indefinitely – because every patient’s feedback about their colonoscopy experience is unique and valuable.
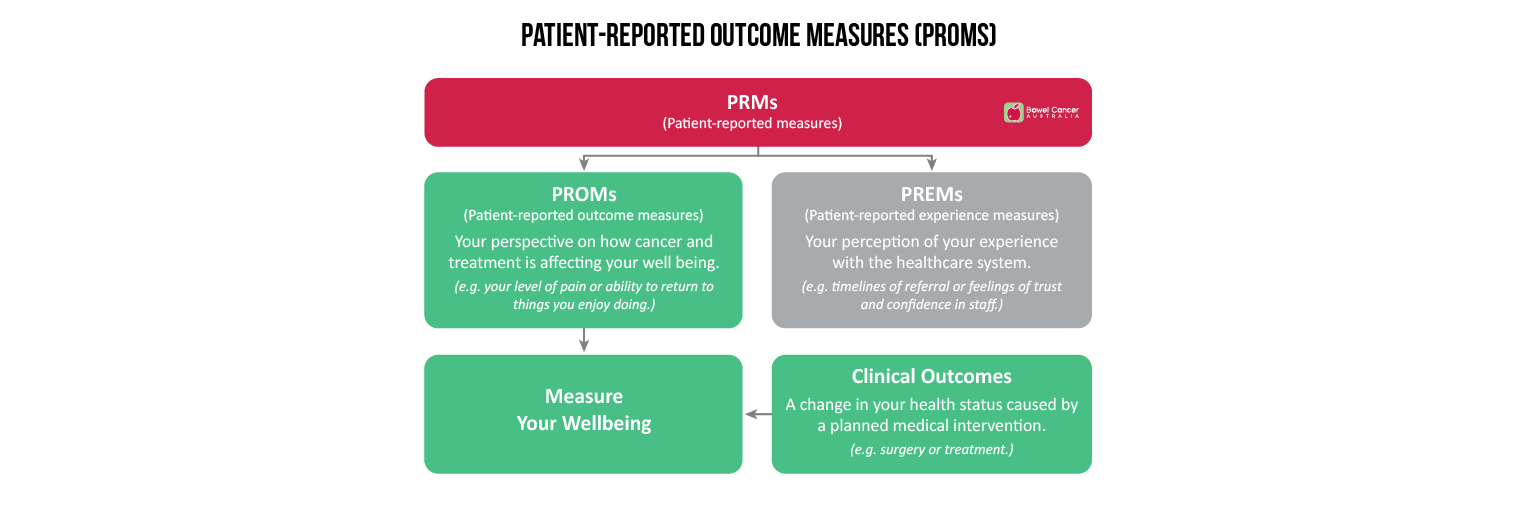
| What are patient-reported outcome measures (PROMs)?
Patient-reported outcome measures (PROMs) are questionnaires that capture the impact disease and treatment is having on a patient's health and wellbeing, from the patient perspective.
By prioritising the concerns patients consider to be most important, PROMs help healthcare professionals detect problems early, address side effects quickly and develop a care plan that supports a patient's specific needs, so they can enjoy the best health possible.
There are two basic types of PROMs -
- General health PROMs can be used to survey patients with any condition. They usually focus on general well-being, mental health and/or quality of life.
- Condition-specific PROMs usually focus on the symptoms of a disease (i.e. bowel cancer). They may ask questions about your mobility, function, or pain levels in certain areas of your body.
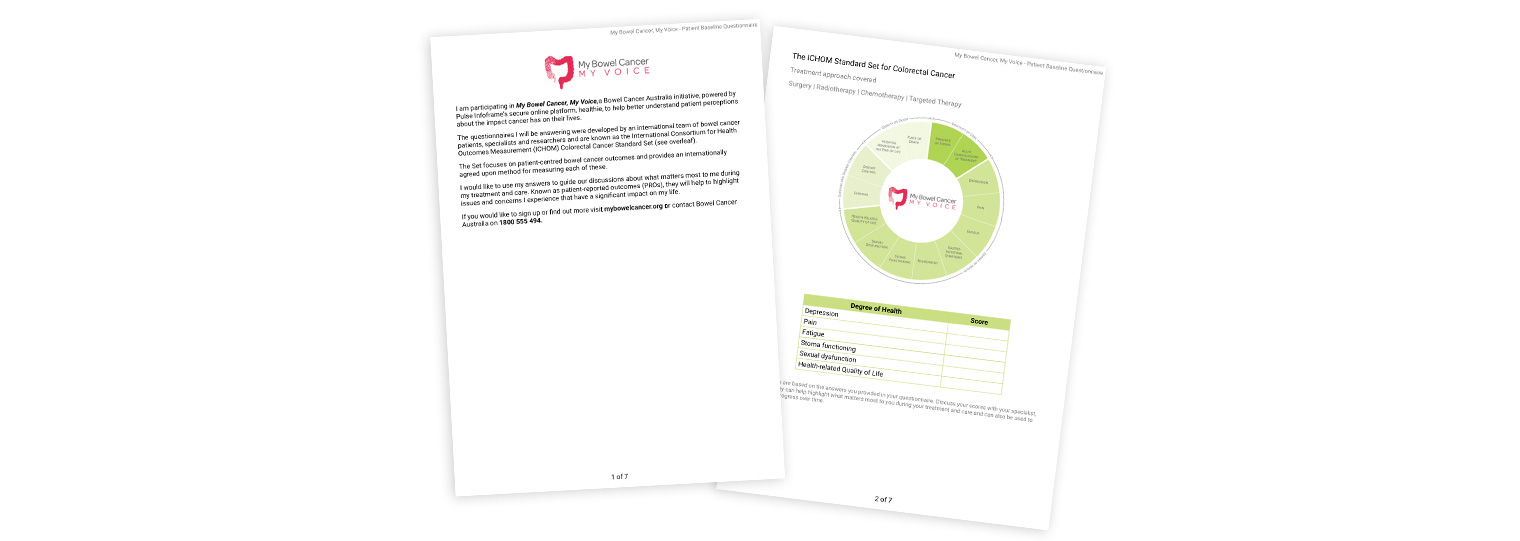
Bowel Cancer Australia’s My Bowel Cancer, My Voice, is a condition-specific PROMs questionnaire.
The answers to these questionnaires are referred to as 'patient-reported outcomes', or PROs.
PROs are patient-centred and relate not just to survival; they address areas affecting the ability to lead a productive life, during and beyond bowel cancer treatment and care.
PROs are reported by the patient, without interpretation of their response by a healthcare professional or anyone else.
The responses are converted into PRO scores which reflect the results a patient cares most about when seeking treatment (e.g. functional improvement and the ability to live a normal, productive life) and create an information-base against which the patient and their healthcare team can monitor and assess progress - before, during and after bowel cancer treatment.
| A global standard in bowel cancer patient care
The ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer was presented for the first time on May 17 at the 2016 ICHOM Conference at University College London, UK.
In a world-first, health professionals, support groups and patient representatives from Europe, Asia, United States and Australia have joined forces to establish and launch a global set of outcomes that reflect the issues that matter most to colorectal (bowel) cancer patients.
The Set of Patient-Centred Outcome Measures for Colorectal Cancer, developed thanks to an international collaboration between Bowel Cancer Australia and the International Consortium for Health Outcomes Measurement (ICHOM), provides the unique opportunity for healthcare providers to share data and learn from one another through one global standard.
“The Set restructures care delivery around value-based outcomes, which has been shown to improve quality of care and curb inefficiencies,” said Professor of Surgical Oncology at Leiden University Medical Center, The Netherlands, Dr Rob Tollenaar, who is presenting the Set of Patient-Centred Outcome Measures for Colorectal Cancer for the first time at the ICHOM Annual Conference in London.
“Measuring, reporting, and comparing health outcomes are among the most important steps toward rapidly improving patient care and reducing costs. By implementing the ICHOM Patient-Centred Outcome Measures for Colorectal Cancer, health providers become part of an expanding, international community of innovative healthcare providers dedicated to improving value for the millions of bowel cancer patients around the world,” he said.
Bowel cancer is the third most common cancer in the world, with around 1.4 million new cases diagnosed each year. It is predicted that this figure will rise to 2.4 million new cases annually worldwide by 2035.
“The ultimate objective of the Patient-Centred Outcome Measures for Colorectal Cancer is to help improve cancer care, leading to better health outcomes for patients,” said Bowel Cancer Australia CEO Julien Wiggins.
“Health professionals are gathering more data than ever before, yet what is measured often has little relationship to the results that matter most to the patients themselves. Led by a team of doctors, researchers, patient support groups and, most importantly, patients from around the world, the Set of Patient-Centred Outcome Measures for Colorectal Cancer becomes a model for global best-practice in patient care.”
Bowel Cancer Australia Patient Ambassador and Former Liberal MP Donna Bauer, one of the patient representatives who helped shape the outcomes contained in the Set of Patient-Centred Outcome Measures for Colorectal Cancer, says long-term care and quality of life were identified among the most important, yet unacknowledged, aspects of patient care.
“Bowel cancer affects people long after the short recovery period from surgery or treatment, and physical and emotional health problems, such as bowel functioning, dietary considerations and anxiety, can remain for the rest of your life. The Set of Patient-Centred Outcome Measures for Colorectal Cancer will facilitate open communication and the sharing of knowledge to help patients in the long-term,” she said.
Australian representatives on the Working Group include: Bowel Cancer Australia, Donna Bauer (Patient Representative and Bowel Cancer Australia Ambassador), Professor John Zalcberg (Monash University), and Professor Craig Lynch (Peter MacCallum Cancer Centre).
For a complete overview of the ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer, including definitions for each measure, time points for collection and associated risk factors, visit Bowel Cancer Australia's online shop.

| The ICHOM Colorectal Cancer Working Group
Long-term health outcomes and quality of life were identified among the most important, yet unacknowledged, aspects of colorectal (bowel) cancer care, according to an international patient survey led by the ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer Working Group. The Working Group is a global collaboration of health professionals, clinicians, patients and consumer health organisations led by Bowel Cancer Australia and the International Consortium for Health Outcomes Management (ICHOM).
In a world-first initiative, more than 200 bowel cancer patient advocates from Australia, North America and Europe, were invited to share their lived experience of cancer, and their perspectives on their treatment and management, to help shape a global standard in care.
The Set of Patient-Centred Outcome Measures for Colorectal Cancer provides the unique opportunity for healthcare providers to share data and learn from one another through one global standard, which is assisting with the implementation of patient-centric best practice guidelines for prevention, diagnosis, treatment and recovery. The aim of the initiative is to develop an international set of outcomes that reflect the issues that matter most to bowel cancer patients.
“Bowel problems are not limited to the short recovery period after surgery or treatment, and the impact of the cancer often remains for the rest of your life,” said Bowel Cancer Australia Patient Ambassador and Former Liberal MP Donna Bauer, who helped develop the ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer.
“There’s a tendency for healthcare professionals to rely too heavily on the short-term benefits and side effects of treatment options. The adoption of an international Set of Patient-Centred Outcome Measures for Colorectal Cancer will facilitate open communication and the sharing of knowledge to help patients with the physical and emotional impact of cancer in the longer-term,” she said.
In the survey, patient respondents also cited overall bowel function, dietary considerations and anxiety and depression, as important factors when assessing quality of life.
“Some patients cannot eat normally again because of the impact of cancer treatment on their bowel function. Always having to check where the toilets are and avoiding places where you can’t go to the toilet immediately is also a major issue for many people,” said Mrs Bauer.
Fear of ostomy, fear of disease progression and concerns about the future were also among the main concerns.
Bowel Cancer Australia, who developed the Set of Patient-Centred Outcome Measures for Colorectal Cancer in consultation with ICHOM and global partners, says the findings are not entirely surprising and the survey reflects the frustration of many bowel cancer patients worldwide.
“Health professionals are gathering more data than ever before, yet what is measured often has little relationship to the outcomes that matter most to the patients themselves. Through the implementation of the Set of Patient-Centred Outcome Measures for Colorectal Cancer, we have a chance to turn this around and adopt a model for global best-practice in patient care,” said Bowel Cancer Australia CEO Julien Wiggins.
"The ultimate objective is to help improve cancer care, leading to better health outcomes for patients."
The adoption of the ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer will enable healthcare providers globally to compare, learn and improve patient care.
"By collaborating with our international partners from North America, Europe and Asia we have a unique opportunity to share data and learn from one another through one global standard," Mr Wiggins said.
"This is particularly important in the Australian context where there is an urgent need to increase our understanding of bowel cancer, particularly in its advanced stages. Data on advanced bowel cancer is not routinely kept in Australia, and we do not know what treatment patients receive, how they respond to this treatment and their level of care," he added.
About the ICHOM Set of Patient-Centred Outcome Measures for Colorectal Cancer
The Set of Patient-Centred Outcome Measures for Colorectal Cancer measures outcomes for patients with newly pathologically diagnosed invasive colorectal cancer (stage I-IV). Key outcomes for measurement, as identified by the Working Group, are categorised according to the following: degree of health; survival and disease control; quality of death; and disutility of care. The following treatment approaches (or interventions) are covered by the Set of Patient-Centred Outcome Measures for Colorectal Cancer: surgery; radiotherapy; chemotherapy; and targeted therapy.
About ICHOM and the Working Group
The International Consortium for Health Outcomes Measurement, or ICHOM, was founded in 2012 by Professor Michael E. Porter of Harvard Business School, the Boston Consulting Group, and the Karolinska Institute. The Set was developed by the ICHOM Colorectal Cancer Working Group, which comprises international leaders and patient representatives across 20 organisations and medical research centres from 10 countries. The Set was co-sponsored by Bowel Cancer Australia, Dutch Institute for Clinical Auditing and Centraal Ziekenhuisgroep (CZ). The standardisation process commenced in July 2015.
The International Consortium for Health Outcomes Measurement, or ICHOM, was founded in 2012 by Professor Michael E. Porter of Harvard Business School, the Boston Consulting Group, and the Karolinska Institute. The Set was developed by the ICHOM Colorectal Cancer Working Group, which comprises international leaders and patient representatives across 20 organisations and medical research centres from 10 countries. The Set was co-sponsored by Bowel Cancer Australia, Dutch Institute for Clinical Auditing and Centraal Ziekenhuisgroep (CZ). The standardisation process commenced in July 2015.